What you need to know about constipation in children?
01.02.2025, by Dr Yik Yee Ian
What you need to know about constipation in children?
Constipation is a symptom and not a disease condition! This symptom has serious consequences and led to many clinic visits and consultations with the paediatrician and paediatric gastroenterologist, at times with referrals to the paediatric surgeon when medical therapies fail. Children with constipation usually have poor quality of life, frequent school absenteeism and low self-esteem.
The symptom of constipation may be part of a clinical syndrome like Hirschsprung disease, Ehlers-Danlos syndrome, Down syndrome etc. It may not be associated with any apparent cause and often labelled as functional constipation by many paediatricians. Constipation may present with difficulty in passing stools, infrequent stools passage, small and hard stools, abdominal pain, bloating, per rectal bleeding and anal pain. At times, it may be associated with fever, vomiting and urinary tract symptoms (e.g. dysuria and urinary retention).
Constipation is defined by Rome IV criteria (must include two or more of the following):
Straining during more than ¼ (25%) of defecations
Lumpy or hard stools (Bristol Stool Form Scale 1-2) more than ¼ (25%) of defecations
Sensation of incomplete evacuation more than ¼ (25%) of defecations
Sensation of anorectal obstruction/blockage more than ¼ (25%) of defecations
Manual maneuvers to facilitate more than ¼ (25%) of defecations (e.g., digital evacuation, support of the pelvic floor)
Fewer than three SBM (spontaneous bowel movement) per week
Clinical assessment of children with constipation will need to determine the presence or absence of faecal impaction and to assess for consequence of chronic obstruction (associated urinary symptoms, failure to thrive, school absenteeism, family burdens, poor quality of life etc).
Common investigations performed in children with constipation include but not limited to:
- AXR (abdominal radiograph): can determine the presence of obstructed bowels and the degree of faecal impaction; serial AXR is used to assess the success of bowel management programme
- USS (ultrasound): to assess the degree of faecal impaction and to assess the urinary tract systems (Kidney, ureter and bladder) for consequence of chronic constipation
- Contrast enema (Figure 1): useful to study the anatomy/ shape of the colon; useful to exclude Hirschsprung disease; can be both diagnostic and therapeutic (for medical disimpaction with gastrograffin enema)
Special investigations are required in children with chronic constipation, not limited to:
- Whole gastrointestinal transit scintigraphy (Figure 2): useful to determine gastric emptying, small bowel transit and colonic transit; 20% of children with chronic constipation will have dysfunctional gastrointestinal transit of the stomach, small bowel and colon; only available in hospital with Nuclear Medicine Department
- Colonic manometry: useful for children with slow colonic transit; invasive study to measure colonic pressure with very few centres capable of performing this study in the world
- Anorectal manometry: invasive study to measure anorectal pressure; useful and diagnostic for dyssynergic defecation and Hirschsprung disease
- Colonoscopy: invasive for assessment and confirmation (with biopsy) of inflammatory bowel disease, i.e. Crohn’s disease and ulcerative colitis
- Magnetic Resonance Imaging (MRI): to detect spina bifida as underlying cause of neuropathic constipation and bladder dysfunction
Management of constipation consists mainly of:
- Non-pharmacological approach
- Lifestyle modification, i.e. active lifestyle with frequent exercises
- Dietary modification, i.e. balanced diets with adequate fiber intake
- Water intake, i.e. adequate hydration to keep stools moist
- Toilet training with proper positioning to ease defecation
- Pharmacological approach, mainly laxatives with subclasses like:
- Bulk-forming laxative, e.g. fybogel, psyllium
- Emollient/ stool softoner laxative, e.g. docusate
- Lubricant laxative, e.g. mineral oil, liquid paraffin
- Stimulant laxative, e.g. bisacodyl, senna
- Osmotic laxative, e.g. polyethylene glycol, glycerin
Mainly by oral routes (a to e) and occasionally by per rectal route, e.g. glycerin enema
- Disimpaction is required in the presence of severe faecal impaction, either by:
- Medical disimpaction:
- High dose laxative by oral route
- Rectal administration of stimulant laxative
- Radiological disimpaction with contrast, e.g. gastrograffin enema
- Surgical disimpaction:
- Rectal and colonic washouts (clinic or ward procedure without sedation/ anaesthesia)
- Rectal digital evacuation / manual disimpaction under general anaesthesia, with rectal and colonic washouts
- Medical disimpaction:
- Neuromodulation therapy
- Sacral nerve stimulation (SNS): invasive; involves implant of a nerve stimulator
- Transcutaneous electrical stimulation (TES): non-invasive; involves use of surface electrodes with administration of interferential currents for stimulation
- Surgery
- Open rectal biopsy: to confirm or exclude Hirschsprung disease
- Colonic biopsy: to determine level of aganglionosis in Hirschsprung disease before definitive surgery (i.e. pull-through procedure)
- Antegrade continence enema (ACE, Figure 3): formation of appendix stoma and to administer antegrade enema to flush out faeces
- Bowel resection (reserved as last option in severe and intractable constipation failed medical therapy): usually of sigmoid colon and sometimes transverse colon, pending assessment of colonic scintigraphy to identify segment of colonic inertia
In children with intractable constipation, a multidisciplinary approach may be needed by a team consists of:
- Paediatrician/ paediatric gastroenterogist/ Bowel dysmotility specialist
- Paediatric Surgeon
- Radiologist
- Nuclear Medicine Physicist
- Dietician
- Physiotherapist
- Stoma therapist
- Continence nurse

Figure 1: Contrast enema in a 2 year-old boy shows faecal impaction (black and round filling defects ) with very redundant sigmoid and transverse colon
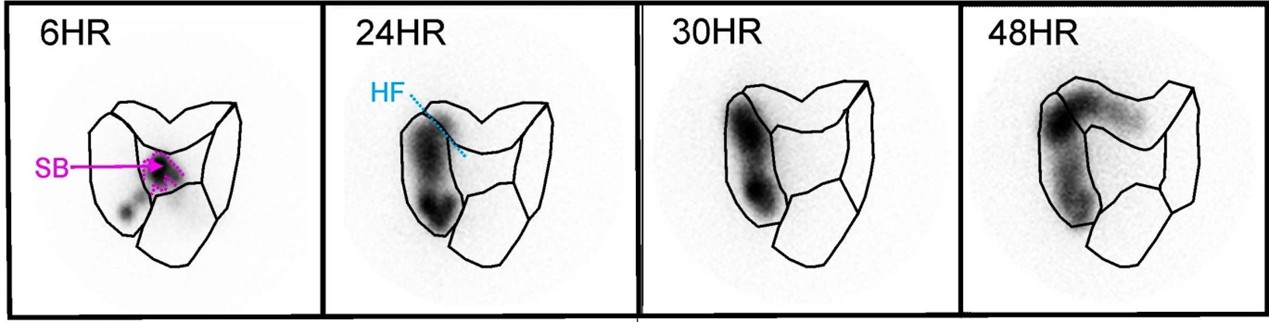 Figure 2: Whole gastrointestinal tract transit study shows slow colonic transit
Figure 2: Whole gastrointestinal tract transit study shows slow colonic transit

Figure 3: ACE stoma for administration of colonic enema to flush out faeces




